2nd EU HCV Policy Summit on the Elimination of Hepatitis C in Europe
Securing sustainable funding for hepatitis elimination plans
Editor-in-Chief, Prof. Angelos Hatzakis MD, PhD
Contents
Note by the Co-Chair of the Hepatitis B &C Public Policy Association, Prof. Angelos Hatzakis MD, PhD
The Hepatitis B and C Public Policy Association (HepBCPPA), is a non-profit organization, which brings together thought leaders and stakeholders from across the board to reflect on recent advances and challenges in understanding, measuring, preventing, diagnosing and treating hepatitis B and C and to develop policy responses that can effectively and measurably address these challenges.
Over the past 9 years, HepBCPPA has organised three high-level meetings and two EU HCV Policy summits in cooperation with the EU Presidency of Belgium, the EU Presidency of Cyprus, the EU Presidency of Greece and European Commission and has instigated and agreed with its partner associations on five Calls to Action addressed to the European Commission and the EU Member States. HepBCPPA also participates in related international and European scientific and policy meetings and lobbies to increase visibility of challenges and the urgency for policy responses.
The introduction of new, safe and effective treatments for HCV in 2013 created an unprecedented opportunity to cure patients and eliminate the disease. However, in the majority of countries HCV elimination represents a serious challenge for countries’ health budgets as they are faced, for the first time in history, with a fast-acting curative high-cost treatment for a widespread, chronic viral disease which offers little risk of resistance or relapse. In addition to treatment costs, the cost of scaling up testing to find the non-identified infected individuals and implementing effective models of care for diverse populations, represent additional challenges.
The economic crisis has impacted on public health spending more than on any other public life sector by shrinking budgets and necessitates austerity, in turn, austerity calls for cuts. Governments are faced with a dilemma: spend now to save later? On what? With what return on investment?
The 2nd EU HCV Policy Summit entitled “Securing sustainable funding for hepatitis elimination plans” was held in Brussels on 6th June 2018. It was a high-level conference and represents the next step organized on the topic of elimination of hepatitis C on a European level. We gathered together the main stakeholders in the field of hepatitis C: clinicians, patient advocacy groups, representatives of key institutions and regional bodies from across Europe to present the case for a European elimination strategy for hepatitis C in the presence of EU and national policymakers.
During the 2nd EU HCV Policy Summit, the case was made for the need to ensure that all elements involved in the cost of HCV elimination – surveillance, monitoring, awareness, screening prevention and treatment programs, are affordable. Preliminary data suggest that the WHO HCV elimination strategy may be cost saving for many countries. That is, the savings related to preventing and treating the long-term consequences of HCV may exceed the cost of HCV elimination, providing good value for money despite the high initial spending. Innovative financing tools include social impact bonds and other tools, with the aim to raise funds upfront for launching new social services and financing prevention services, including harm reduction, thus contributing to HCV elimination in a sustainable way. Some European countries have significant experience in creating social bonds and similar financing tools. Others may prefer to explore other opportunities through cooperation with the European financial institutions such as the European Investment Bank. As George Papandreou, President of Socialist International and former prime minister of Greece, emphasized, “experts, patients and stakeholders need to campaign and inform the European Parliament, the EU Commission as well as national governments” regarding this tremendously important message.
Strategic Direction 4 of the WHO Global Health Sector Strategy on Viral Hepatitis 2016-2021 “Financing for Sustainability” sets out financing recommendations for a sustainable hepatitis response, outlining actions to raise revenue to pay for viral hepatitis interventions and services, set up financial risk protection, and improve efficiency in the use of health system resources. In this regard, George Papandreou, Prof Jagpreet Chhatwal and others suggested the idea of creating social bonds and similar financing tools through cooperation with the European financial institutions such as the European Investment Bank.
The European institutions and stakeholders represented at the summit were the European Parliament, represented by the Co-Chair of the Friends of the Liver MEP group, Dr Cristian-Silviu Busoi, Dr. Antons Mozalevskis (WHO Europe) the European Liver Patients’ Association and chair of ACHIEVE Coalition, Dr Tatjana Reic, Educational Councillor of the European Association for the Study of the Liver, Prof Francesco Negro, the CORRELATION Network & European Civil Society Forum, Mr. Eberhard Schatz.
In addition, the summit was attended by several members from national Parliaments (e.g. Ricardo Baptista-Leite, Portugal, Kostas Bargiotas from Greece and Zeliko Jovanovic from Croatia). Ninety delegates attended the event. Twenty-nine nationalities were present including Austria, Belgium, Bulgaria, Canada, Croatia, Denmark, Egypt, France, Germany, Greece, Hungary, Ireland, Israel, Italy, Latvia, Lithuania, Macedonia, Malta, The Netherlands, Portugal, Romania, Slovakia, Slovenia, Spain, Switzerland, Turkey, Ukraine, United Kingdom and the USA.
The launch of the Call to Action with its 7 points provides a road map for action.
This issue of Hepatitis B and C Public Policy Association’s newsletter is dedicated the 2nd EU HCV Policy Summit. We invite you to read the meeting summary, share your thoughts with us and join in the effort to raise the bar for management of viral hepatitis in Europe.
Angelos Hatzakis MD, PhD
Co-Chair, Hepatitis B and C Public Policy Association
Professor of Epidemiology and Preventive Medicine
Department of Hygiene, Epidemiology and Medical Statistics
Athens University Medical School
Athens
Greece
Email: [email protected]
“Securing sustainable funding for hepatitis elimination plans”
1. Introduction
The 2nd EU HCV Policy Summit entitled “Securing sustainable funding for Hepatitis C Virus elimination plans” took place in Brussels on 6th June 2018 bringing together high-level policy makers and academics, patient advocates, health organisations and other stakeholders. Prof. Angelos Hatzakis (Greece) and Prof Michael Manns (Germany), Co-Chairs, Hepatitis B&C Public Policy Association, introduced and welcomed the participants emphasizing the importance of sustainable funding for hepatitis C (HCV) elimination particularly among European countries where differences in financing and insurance systems is a major challenge. Dr. Tatjana Reic, President of the European Liver Patients Association (ELPA), and Co-Chair of ACHIEVE Coalition, mentioned the importance of political support and the need for national strategies for elimination of hepatitis C, while Dr. Cristian-Silviu Busoi, Member of the European Parliament and Co-Chair of the Friends of the Liver MEP Group, emphasized that elimination of hepatitis C should be placed higher in the European Union’s (EU) agenda as an urgent health priority, while efforts should be undertaken for successful negotiation and more flexible agreements with the pharmaceutical industry. Prof. Francesco Negro, European Association for the Study of the Liver (EASL), Switzerland, reported in his introduction, that the epidemiology of hepatitis C in Europe is fairly well characterized: it is estimated that one third has been diagnosed, but too few have been treated. DAAs are now available -without restrictions- in most major Western European countries and prescribed by specialists according to the EASL guidelines. However, during recent years, migration is a challenge, since about 2.1 million migrants are estimated to be anti-HCV positive, with 30,000 new arrivals of migrants every year. Another challenge is hepatitis C in Eastern Europe, since currently there is an epidemic exploding driven by intravenous drug use, the absence of surveillance systems, national strategies, limited or no funding for hepatitis programs and the lack of awareness at all levels (especially political).
2. Burden of disease and pathways of elimination
HCV elimination in Europe: Burden pathways and cost
As Dr. Homie Razavi (USA) presented, 3 million people are infected with hepatitis C in the EU, and of these, 68% are undiagnosed and less than 6% have been treated. In addition, despite the availability of curable therapies with DAAs, 16,000 patients were diagnosed with hepatocellular carcinoma and 22,500 deaths related to chronic hepatitis C were recorded in 2017, i.e. every 25 minutes, an HCV infected person died of liver complications in the EU in 2017. The cost of inaction is great – 136,000 additional deaths, 90,000 additional HCC cases, and 71,000 decompensated cirrhosis cases are estimated between 2017-2030.
Fortunately, the actual number of treated patients with hepatitis C has increased over the last few years since DAAs became available and the EU only needs to diagnose 160,000 (from today’s 90,000) and treat 180,000 (from 160,000 today) annually to reach the 2030 WHO elimination target. However, even EU countries with a high treatment rate will not be able to sustain the treatment without universal screening, while political will is the main predictor of whether a country will achieve the 2030 elimination targets.
Currently, only a few countries in the world (Australia, Egypt, Georgia, Iceland, Italy, Japan, Mongolia, Netherlands, Spain, Switzerland, UK and France), are on track for HCV elimination by 2030. In order to achieve these elimination targets seven requirements are needed: 1) financing of national elimination programs, 2) implementation of harm reduction programs, 3) expanding capacity beyond specialists, 4) removing treatment restrictions, 5) implementing monitoring & evaluation, 6) implementing awareness and national screening programs, 7) implementing national linkage to care program.
The micro-elimination approach to eliminating hepatitis
Prof. Jeffrey V. Lazarus (Spain) mentioned that the WHO Global Sector Strategy on viral hepatitis set the following targets at two time points (2020 and 2030): a) incidence: reduction by 30% at 2020 and by 80% at 2030, b) mortality: reduction by 10% at 2020 and by 65% at 2030, c) harm reduction: increase in sterile needle and syringes provided per PWID/year from 20 in 2015 to 200 at 2020 and 300 at 2030, d) testing: 90% of people aware of HCV infection at 2030 and e) treatment: 80% of people treated by 2030.
These WHO targets for HCV elimination are challenging, costly and complex. However, the continuum of viral hepatitis services and the retention cascade need simplification similar to those of HIV infection considering that every country may have different barriers to overcome. In addition, it should be recognized that although the cost is falling on several levels (diagnosis, treatment etc.), elimination of hepatitis C is still daunting for the health system. However, an idea is to break down this cost by subgroup of population, by year, by region etc. In fact, formidable obstacles to reaching HCV elimination can best be overcome through a micro-elimination approach, which entails pursuing elimination goals in specific populations through multi-stakeholder initiatives that tailor interventions to the needs of these populations. Micro-elimination is less daunting, less complex, and less costly than full-scale, country-level initiatives to eliminate HCV, and it can build momentum by producing small victories that inspire more ambitious efforts.
WHO-EURO: progress report
To reinforce the commitment of the global goal, members of the EU have endorsed the first European action plan, which is in line with the global strategies including five strategic directions: information for focused action, interventions for impact, delivering for equity and innovation for acceleration. Based on this plan, several regional essential targets should be reached by 2020 regarding prevention (harm reduction), and particularly, testing and treatment. Dr. Antons Mozalevskis (WHO Europe) reported that for an effective and coordinated response the global health sector strategy and regional action plans should be translated into national strategies or plans. It is encouraging that the number of European countries with national plans increased from 13 in 2013 to 22 in 2017. However, several challenges remain, since there is a lack of global donors and commitment in many countries, data is patchy and monitoring systems are nascent, most people living with hepatitis are still undiagnosed, treatment access is limited by regulatory barriers and high prices (particularly for newer antiviral drugs), while addressing vulnerable / key populations can be a political issue. Of course, one of the most important barriers is the cost of HCV elimination programs.
Barriers for HCV elimination
Prof. Mojca Maticic (Slovenia) mentioned that several barriers and gaps in the cascade-of-care should be overcome from the side of patient, the health system and of course the policy and solutions need to be found and subsequently funded. All stakeholders and decision makers should work together and collaborate in order to achieve the necessary scale-up for hepatitis C elimination. This aim is very ambitious and there is an urgent need to improve the services and to reach and understand the specific characteristics (culture, language etc.) of each subgroup, e.g. immigrants, MSM, PWIDs. Hence, the WHO recommends the member states to devise a national plan and guidelines, but on an individual level, the most important issue seems to be the simplification of existing models of care.
3. The cost of HCV elimination
Cost of HCV elimination: Direct medical cost, patients reported outcomes and productivity loss
Dr. Zobair Younossi (USA) emphasized that Patient-Reported Outcomes (PROs) and Work Productivity (WP), both important components of comprehensive outcomes assessment, are impaired in HCV infected patients. PROs are important surrogate markers of patient experience, and their impairment, especially in the domains of physical functioning and mental health, is the result of the virus replication itself. Regarding WP, HCV appears to affect absenteeism and presenteeism from work leading to substantial economic burden to employers. As a result, although in 2011 the total direct cost of HCV-related liver disease was estimated at 6.5 billion USD in the USA (projected to peak at 9.1 billion in 2014), the indirect economic burden of WP loss in the USA has been estimated to be approximately 7.1 billion USD per year and 2.6 billion Euros per year in 5 major European countries (France, Germany, Spain, Italy and United Kingdom).
Cost of screening
HCV screening guidelines still target only people at high risk of infection, but this approach requires reconsideration in the light of new and more effective antiviral treatments with DAAs, which can be used as a means of prevention, particularly in high-risk populations, such as MSM and PWIDs. Although there is great heterogeneity across European countries, the need to improve HCV screening is widespread (e.g. in France 100,000 people have chronic hepatitis C and half of them are undiagnosed in 2018). Interestingly, Prof. Sylvie Deufic-Burban (France) assessed five different mathematical models regarding effectiveness, cost and cost-effectiveness in France, showing that universal (100%) screening coverage plus treatment initiation regardless of fibrosis stage (i.e. from fibrosis F0) can reduce the prevalence of HCV by 94% after one year, compared to 40% reduction with 50% screening coverage plus treatment initiation regardless of fibrosis stage. In addition, with 50% screening coverage plus treatment initiation regardless of fibrosis stage, the incidence of compensated HCV cirrhosis will be reduced by 30% after ten years. In addition, the model of universal (100%) screening coverage plus treatment initiation regardless of fibrosis stage seems to be cost-effective (31,100 €/QALY), but in contrast, it is not cost-effective if treatment is given only to those with fibrosis ≥F2.
Price tag for bringing hepatitis B and C services under the umbrella of Universal Health Coverage
Efficient allocation of resources elimination is a cornerstone of the Global Hepatitis Strategy and, as Dr. David Tordrup (WHO advisor UK), proposed, this can be achieved by: a) increasing efficiencies (i.e. reduction of budget impact) with high impact interventions, simplified management, adopting strategies of price reduction in diagnosis and medicine and improving service delivery, and b) identifying financing solutions (i.e. inform resource allocation) using external and internal funding, innovative financing and fair allocation of budget.
Is hepatitis C elimination cost-saving?
Prof. Jagpreet Chhatwal (USA) mentioned that in the USA, DAAs treatment can reduce the burden of HCV-associated disease by 50% -70% between 2015 and 2050: liver-related deaths (from 767,000 without treatment to 317,000), hepatocellular carcinoma (from 407,000 without treatment to 154,000) and liver transplants (from 63,000 without treatment to 31,000).
Although the prices of antiviral therapies increase over time, the costs for cure decrease steadily over time because more effective therapies are available. Interestingly, the life-time cost of hepatitis C treatment using DAAs is less than <30,000$ (particularly with the implementation of generic drugs), significantly lower than HIV treatment (315,000$) and primary biliary cholangitis using obeticholic acid (900,000$).
It was shown from data in the UK, where keeping the current status quo, it is estimated that the total cost (natural history, diagnosis and treatment) over the next twenty years is about 11.7 billion dollars, compared to 10 billion dollars with elimination scenario (i.e. saving 1.7 billion dollars). Resources spent on HCV elimination provide good value for money and will result in cost-savings. Thus, HCV elimination is feasible and will save lives. However, great initial investment is needed to eliminate HCV.
4. Innovative financing
Innovative financing of HCV elimination
It is true that for HCV elimination, investment is needed over a long period of time (e.g., providing antiviral treatment until 2030). Prof. Jagpreet Chhatwal mentioned that financial bonds could provide a mechanism to raise funds to eliminate HCV, since the more we treat, the more lives saved and more economic savings. Bond finance can be used to effectively transfer the risks associated with long-term spending commitments from governments to investors. Through bond finance, not only can governments release money for public spending, but the maturity period can be adjusted to the timeframe in which the investment produces the desired social/economic benefit. One option could be commercial bonds, which are widely used in the public sector for funding infrastructure projects like roads, schools and bridges, and other “social investments”. In this category, green bonds used to fund a variety of local enterprises and initiatives that can contribute to “green” projects (e.g., renewable energy, clean water), while vaccine bonds were developed by the International Finance Facility for Immunization (IFFIm). The latter was created by France, the UK and other European countries in 2006 to provide vaccines to raise finance for the GAVI Alliance. Another option could be the Social Impact bonds, i.e. a contract with the public sector in which a commitment is made to pay for improved social outcomes that result in public sector savings (e.g., social bond for rehabilitation of incarcerated people and to reduce recidivism). Based on these experiences, the establishment of a “HCV bond” could be an effective and realistic option to finance hepatitis C elimination.
Financing solutions for hepatitis elimination in low and middle-income countries
Although hepatitis elimination has a positive return on investment– the main problem is the need for upfront investment. Dr. Homie Razavi (USA) suggested that one approach could be based on patients who are willing to pay for healthcare expenses (for example in many of the lower middle-income countries a high proportion of patients of all treatments are currently in the private market) providing that the costs are kept below the catastrophic healthcare expenditure level, while some portion of the population will not be able to pay for their healthcare. This model can be supported by suppliers who are willing to provide price concessions if large volumes are guaranteed, as well as banks and donors who are willing to provide catalytic financing if they have assurances that can get their investment back at the end of the program.
The new model would foresee the use of loans instead of donations to support the hepatitis elimination programs. Thus, although the old model based on donations (donations from the few pay for the needs of the many, including for those who could afford some payment), in the proposed new model, patients fund their treatment (small loan from investor, plus funds from many patients, pay for diagnostics and treatment for all, plus repayment to investor).
5. Opportunities and challenges
Dr. Tatjana Reic, President of the European Liver Patients Association, and Co- Chair of ACHIEVE Coalition, stated that more efforts are needed to raise awareness of viral hepatitis amongst the population and to improve diagnosis of HCV in primary care settings providing sustainable, affordable, universal access to the tools for elimination. It is important to build on support of the European Parliament and to influence the agenda of the next European Commission and the governments of EU Council Presidencies during the transition 2019-2020 aimed to improve diagnosis and access to treatment amongst defined key groups, such as PWIDs.
Eberhard Schatz, Coordinator, CORRELATION network & European Civil Society Forum emphasized the need to move towards a single-visit hepatitis C diagnosis, instead of the current five visits in order to decrease the time of diagnosis and the rates lost to follow up. The new treatment options should be provided in community settings, since hospital attendance requirements are evidenced barriers for marginalized populations. In this direction, more efforts are needed to increase screening in risk groups and build capacity for treatment.
Political leadership may play an important role to deliver the message of hepatitis C elimination at political level keeping hepatitis C high on the political and media agendas Dr. Ricardo Baptista-Leite, Member of Portuguese Parliament, proposed an organized network of Parliamentarians, in order to increase their involvement in international – multilateral workgroups and decision processes aiming to reboot the political awareness and action towards elimination of hepatitis C. He presented the goals of Portuguese Programme for HCV elimination.
6. Conclusions
The Call to Action of the 2nd EU HCV Policy Summit recommends that countries have a comprehensive, costed hepatitis C elimination strategy in place, to determine their country-level disease and economic burden of HCV by measuring direct and indirect socio-economic costs to improve the response towards HCV elimination and to develop country and population-specific models, as viral to estimate lifetime costs, quality-adjusted life expectancy, and incremental cost-effectiveness ratios of different screening and treatment strategies with comparison with no action. These are necessary to hepatitis elimination programs as hepatitis investment cases.
Innovative financing tools include social impact bonds and other tools, with the aim to raise upfront funds for launching new social services and financing prevention services, including harm reduction, contributing to HCV elimination in a sustainable way. Some European countries have significant experience in creating social bonds and similar financing tools. Others may prefer to explore other opportunities through cooperation with the European Financial Institutions such as the European Investment Bank.
The European Union should recognize the need to engage in HCV elimination by establishing a clear political roadmap and call for European financial institutions to raise public or private funding and use elimination programs as development tools. Encourage and engage all the stakeholders to collaborate in the development of innovative financing tools like social impact bonds.
George Papandreou, President of the Socialist International, former Prime Minister of Greece and keynote speaker of the 2nd EU HCV Policy Summit commended: “At a time of Euroscepticism, a time where the value of our Union is put into question both by internal political forces and external players, a project such as this one highlights the added value of a European Union. A Union with the political will and the capacity to change the lives for the betterment of so many of our citizens”.
To view presentations of the summit please visit the HepBCPPA summit website: www.hcvbrusselssummit.eu
Background
The hepatitis C virus (HCV) is a global public health threat with significant morbidity and mortality. Due to its asymptomatic nature, it is also a silent epidemic with an estimated 71 million infected globally, but only 20% diagnosed (1,2).
In 2013, the introduction of new, safe and effective treatments for HCV created an opportunity to eliminate the disease. However, in some settings, this development represents a serious challenge for countries’ health spending as they are faced, for the first time in history, with a fast-acting curative treatment for a widespread chronic viral disease which offers little risk of resistance or relapse. In addition to treatment costs, the cost of scaling up testing to find the non-identified infected individuals and implementing effective models of care for diverse populations, represent an additional challenge.
Greater efforts are needed to ensure that all elements of cost of HCV elimination, which include surveillance, monitoring, awareness, screening, prevention and treatment programs, are affordable. Preliminary data suggest that the WHO HCV elimination strategy may be cost-saving for many countries (3, 4). That is the savings related to preventing and treating HCV may exceed the cost of HCV elimination, providing good value for money given the high initial spending. Strategic Direction 4 of the WHO Global Health Sector Strategy on Viral Hepatitis 2016-2021 “Financing for sustainability” (5) sets out financing recommendations for a sustainable hepatitis response, outlining actions to raise revenue to pay for viral hepatitis interventions and services, set-up financial risk protection, and improve efficiency in the use of health system resources.
On 17 February 2016, the launch of the HCV Elimination Manifesto “Our vision for a Hepatitis C-free Europe”, provided a starting point for action to make HCV and its elimination in Europe an explicit public health priority (6, 7). With patients, civil society groups and other relevant stakeholders directly involved in developing and implementing HCV elimination strategies, now is the time to take the next step further and make the HCV elimination affordable.
We, the signatories of the Call to Action “Secure sustainable funding for hepatitis C elimination plans” are committed to HCV elimination in Europe.
In line with the 2015 United Nations’ General Assembly Resolution “Transforming our world: the 2030 Agenda for Sustainable Development”, in line with the Sustainable Goal 3 Good Health and Well-Being and its Target 3.3 to Fight Communicable Diseases, in line with the 2014 World Health Assembly’s Resolution 67.6 on hepatitis, in line with the 2016 HCV Elimination Manifesto, in line with the WHO Global Health Sector Strategy on Viral Hepatitis 2016-2021 “Towards ending viral hepatitis”, and in order to encourage policy-makers to fulfil the Strategic Direction 4 of the WHO Global Health Sector Strategy on Viral Hepatitis 2016-2021, and make HCV elimination affordable, we are calling on the European decision makers to:
-
Ensure that countries have a comprehensive, costed hepatitis C elimination strategy in place, including a comprehensive monitoring along with the cascade of care in line with the criteria developed by ECDC and WHO Europe;
-
Determine their country-level disease and economic burden of HCV by measuring direct and indirect socio-economic cost to improve the response towards HCV elimination, paying attention to the close link between HCV and HIV in some populations;
-
Develop country and population-specific models, as viral hepatitis investment cases, to estimate lifetime costs, quality-adjusted life expectancy, and incremental cost-effectiveness ratios of different screening and treatment strategies with comparison with no action;
-
Allocate sufficient resources for training and research, developing robust models of care for tackling HCV, and urgently and effectively fulfil Strategic Directions 2, 4 and 5 of the WHO Global Health Sector Strategy;
-
Recognise the need for the European Union to engage in HCV elimination by establishing a clear political roadmap and call for European financial institutions to raise public or private funding and use elimination programs as a development tool;
-
Encourage and engage all the stakeholders to collaborate in the development of innovative financing tools like social impact bond and others, with the aim of launching new social services and financing prevention services, including harm reduction, contributing to HCV elimination in a sustainable way;
-
Exchange and implement best practices on funding healthcare and HCV elimination, including via micro-elimination approaches (8), at the national, regional and local levels to meet the WHO elimination goals by 2030 and preferably much earlier.
References
- WHO Global Hepatitis Report 2017.
- The Polaris Observatory HCV Collaborators. Global prevalence and genotype distribution of hepatitis C virus infections in 2015: a modelling study. Lancet Gastroenterology Hepatology 2017 Mar,2(3):161-176.
- Kondili L et al. Modeling cost-effectiveness and health gains of a “Universal” versus “Prioritized” hepatitis C virus treatment policy in a real-life cohort. Hepatology 2017 Dec;66(6):1814-1825.
- Chhatwal J. “Is hepatitis C elimination cost saving?” 2nd EU HCV Policy Summit, Brussels 2018.
- Global Health Sector Strategy on viral hepatitis 2016-2020. WHO, 2016.
- Action plan for the health sector response to viral hepatitis in the WHO European region. WHO, 2017.
- Papatheodoridis G. V. et al. Summit review: HCV Policy Summit Hepatitis C: The Beginning of the End Key elements for successful European and national strategies to eliminate HCV in Europe, Journal of Viral Hepatitis, Volume 25, Issue S1, 2018
- Lazarus JV, Wiktor SZ, Colombo M, Thursz M on behalf of the EASL International Liver Foundation. Micro-elimination – a path to global elimination of hepatitis C. Journal of Hepatology, July 2017.
George Papandreou, President of Socialist International and former prime minister of Greece.
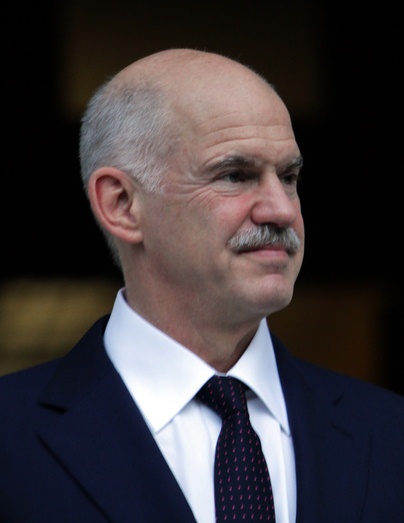 I am honoured to address the EU HCV Policy Summits organized by the Hepatitis B and C Public Policy Association, for a second time.
I am honoured to address the EU HCV Policy Summits organized by the Hepatitis B and C Public Policy Association, for a second time.
I understand that both hepatitis C virus infection and chronic hepatitis C are a public health hazard. Morbidity and mortality are significant in Europe and globally.
Yet new safe and effective treatments can cure chronic hepatitis C. This indeed is a remarkable achievement. It represents an historic opportunity, not only to cure those infected, but also to eliminate this disease globally.
The World Health Organization has affirmed this possibility by adopting the Global Health Sector Strategy to eliminate HCV by 2030. So, we face both a challenge and a huge responsibility.
To succeed, we need both good diagnostic practices and delivery of treatment for those who are infected.
I am thrilled to hear that there has been great progress on both fronts, complemented by price reductions in treatment and affordable diagnostics.
Still, the total cost of surveillance, awareness campaigns, screening, prevention and treatment remains too costly for many around the world. Not surprisingly, the economic burden is especially high for the EU countries.
Investing for the improvement of health is however not only a morally correct thing to do but it yields social and economic benefits.
What is however a crucial fact this Summit has highlighted -a fact that policy and decision makers need to seriously consider- is that the cost of elimination is lower than the cost of treating the long-term consequences of HCV, such us chronic hepatitis, cirrhosis and liver cancer.
So, investment towards HCV elimination not only provides cure from suffering but is also the best value for money.
We know of course that the upfront investment will be high.
Experts, patients and stakeholders need to campaign and inform the European Parliament, the EU Commission as well as national governments.
The message is that HCV elimination programs are highly cost-effective, cost-saving and life-saving.
I had the opportunity in the previous Summit, to outline how European financing institutions could be induced to prepare financing tools and support national HCV elimination programs for the European countries.
I am glad to see that a major part of the analytical work has been finalized and the conclusions are presented here during today’s Summit.
Some European countries, have important experience in creating social bonds and similar financing tools. Others may prefer to explore opportunities through cooperation with the European Financial Institutions such as the European Investment Bank.
So, I would suggest that the next crucial step now, is for the EU Commission to prepare the legislative actions, to convincingly motivate the European Investment Bank and other European financial institutions to take this ambitious yet totally realistic project on board.
At a time of Euroscepticism, a time where the value of our Union is put into question both by internal political forces and external players, a project such as this one highlights the added value of a European Union. A Union with the political will and the capacity to change the lives for the better of so many of our citizens.
I can only conclude by congratulating you all, in this 2nd EU HCV Policy Summit on “Securing sustainable funding for Hepatitis C Virus elimination plans”.
I offer my wishes, and all my support for the best of success
George A. Papandreou